Collapsed Lung (Atelectasis)
Overview
The lungs are like a pair of balloons inside the chest that fill up with air and then relax to let air leave the body. When a blockage occurs in the airway so the lung cannot fill up with air or if a hole or weakened place develops in the lung allowing air to escape, the lung can collapse like a balloon that has lost its air.
Symptoms
Symptoms of a collapsed lung vary. They may include:
- Falling oxygen levels in the blood, which causes the person to look bluish or ashen and can bring on abnormal heart rhythms (arrhythmias)
- Fever if an infection is present
- Rapid, shallow breathing
- Sharp pain on the affected side, if the symptoms are severe and the blockage occurred quickly
- Shock with a severe drop in blood pressure and a rapid heart rate
- Shortness of breath, which can be sudden and extreme in severe cases
If the blockages happen slowly, there may be few or no symptoms. Those that do occur may include shortness of breath, an increased heart rate or a hacking cough that does not seem to go away.
Causes and Risk Factors
A collapsed lung is often the result of pressure on an airway from outside - a swollen lymph node or fluid between the lining of the lungs and the chest wall, for example - can also cause a lung to collapse.
When the airway is blocked, the blood absorbs the air inside the air sacs (alveoli). Without more air, the sac shrinks. The space where the lung was before the collapse fills up with blood cells, fluids and mucus. It may then become infected.
Other factors can lead to a collapsed lung include:
- A plug of mucus, a tumor or something breathed into the lungs.
- Abdominal swelling
- Experiencing high speeds, such as being a fighter jet pilot
- Injuries, such as from a car accident, a fall or a stabbing
- Lack of the liquid (surfactant) that coats the lining of the alveoli, which helps keep it from collapsing. This can happen in premature babies or in adults who have had too much oxygen therapy or mechanical ventilation.
- Large doses of opioids or sedatives
- Lying immobilized in bed
- Scarring and shrinking of the membranes that cover the lungs and line the inside of the chest, which can occur as a result of exposure to asbestos
- Smoking
- Surgery, especially involving the chest or abdomen
- Tight bandages
Diagnosis
To diagnose a collapsed lung, a physician conducts a physical examination and asks about symptoms and the setting in which they occurred. Other tests that may be performed include:
- Bronchoscopy
- Chest X-rays, which may or may not show the airless area of the lung
- Computed tomography (CT), which can help identify an obstruction
Treatment
There are several options for treating a collapsed lung. For example:
- If the lung has collapsed because of a blockage, the blockage can be removed by coughing, suctioning the airways or bronchoscopy
- Antibiotics can be given to treat an infection
- Surgery to remove a part of the lung may be needed if chronic infections become disabling or if significant bleeding occurs
- Surgery, radiation, chemotherapy or laser therapy may be used if a tumor is causing the blockage
- Drugs to treat a lack of surfactant. This is a life-saving measure in newborns. In adults with acute respiratory distress syndrome, it is considered experimental. For adults, the amount of oxygen in the blood is raised by continuous positive-pressure oxygen or mechanical ventilation.
Prevention
Preventing a collapsed lung is as important as treating one. These help avoid a collapsed lung:
- Patients who smoke should stop six to eight weeks before surgery
- After surgery, patients should breathe deeply, cough regularly and move about as soon as possible. Certain exercises, such as changing positions to help the lungs drain, or devices to encourage voluntary deep breathing (incentive spirometry) also help.
- Patients with a deformed chest or nerve condition that causes shallow breathing might need help breathing. Continuous positive airway pressure delivers oxygen through the nose or a facemask. This ensures the airways do not collapse even during the pause between breaths. Sometimes a mechanical ventilator is needed.
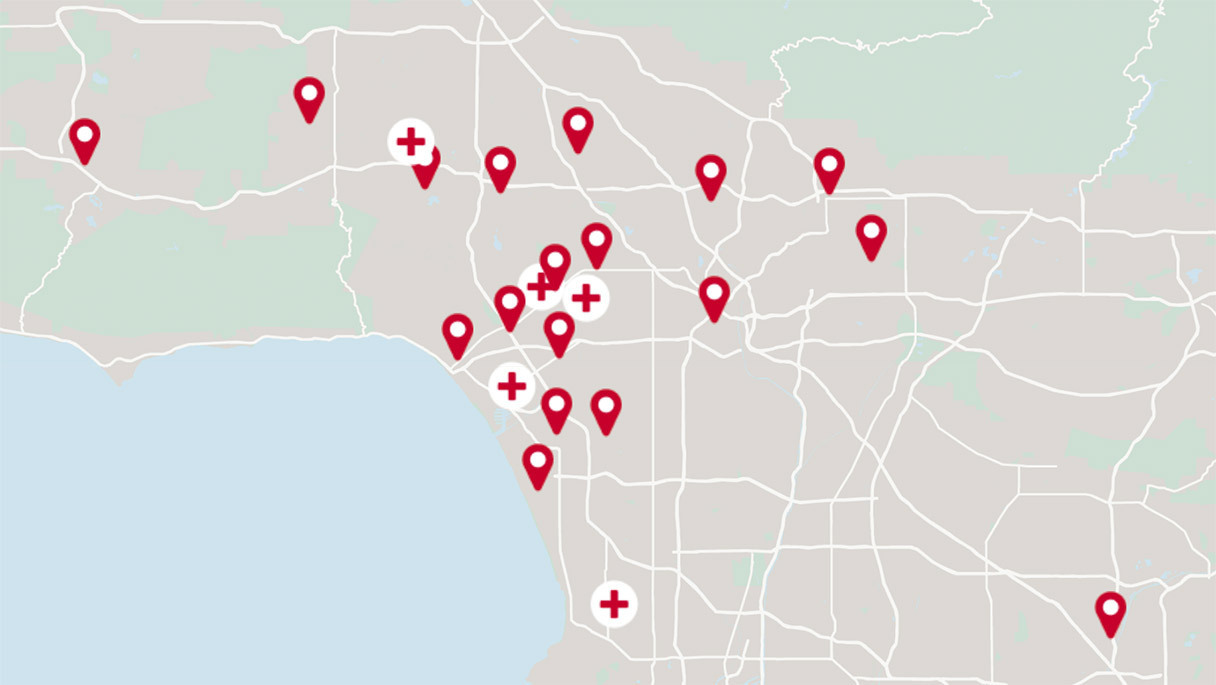
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.