Epilepsy
Overview
Epilepsy is a disorder of the nervous system. Epilepsy causes sudden, intense bursts of electrical activity in the brain. These bursts cause seizures, which may affect:
- Muscle control
- Movement
- Speech
- Vision
- Awareness
Someone with epilepsy will have repeated seizures. There is often no warning and no clear reason why the seizures happen. If epilepsy is not treated, seizures may occur throughout a person's life. Seizures can become more severe and happen more often over time.
Epilepsy can be caused by tumors or improperly formed blood vessels. Epilepsy is broken into three categories based on where the disruption in the brain occurs that triggers the seizure:
- Mesial temporal lobe epilepsy. This part of the brain controls emotions, short-term memory, and the fight-or-flight response. This is the most common form of epilepsy.
- Mesial frontal lobe epilepsy. This epilepsy starts in the part of the brain that controls movement, speech, judgment and problem solving. It is the second most common form of epilepsy. It often causes partial seizures.
- Other extratemporal lobe epilepsies. This includes epilepsy that starts in any other part of the brain, including those that control sensory information, visual information, language, math and other functions.
Symptoms
People with epilepsy may have general seizures, which affect the entire surface of the brain, or partial seizures.
Partial seizures begin in a specific area in the brain. They are also called focal seizures. These seizures may affect only one part or one side of the body. The area affected will depend on where in the brain the seizure happens.
Some symptoms of partial seizures include:
- Jerky or rhythmic movements
- Sensations such as tingling, dizziness, feeling full in the stomach
- Repetitive motions
- Staring
- Confusion
- Changes in emotions
- Altered senses
Generalized seizures may affect all areas of the body.
Some symptoms of generalized seizures include:
- Convulsions
- Crying out or making a noise
- Stiffening
- Jerky, rhythmic or twitching motions
- Falling down
- Loss of consciousness
- Not breathing
- Confusion after returning to consciousness
- Loss of bladder control
- Biting the tongue
Causes and Risk Factors
In most cases, there is no known cause of epilepsy. However, several factors may be at play in the onset of the condition, such as:
- Serious head injury
- Stroke
- Brain tumor
- Brain infection (meningitis or encephalitis)
- Alzheimer's disease
- Loss of oxygen at birth
- Hardening of the brain's arteries
Children are more likely than adults to develop epilepsy. The reason for this is not known. A family history of epilepsy may sometimes be a factor. Experts are not sure how the disease is passed from parent to child.
Not all seizures are caused by epilepsy. They may be caused by injury, illness or other medical conditions. In these cases, seizures end when the condition improves or heals.
Diagnosis
Diagnosing the type of epilepsy a person has, and if their seizures are caused by epilepsy. Your doctor will want to know details of your seizure, such as how long it lasted, what symptoms you experienced, and what parts of your body were affected.
A detailed medical history is also an important part of making a diagnosis.
The most useful way to diagnose epilepsy is an electroencephalogram (EEG). This records electrical activity in the brain. The EEG can record unusual spikes or waves in electrical activity patterns. Different types of epilepsy can be identified with these patterns.
Video EEG monitoring can be used to record seizures on a digital video recording. This allows the doctor to see what happens just before, during and right after a seizure. The video records what the body is doing, and the EEG records the electrical activity occurring in the brain. Such monitoring may be used prior to surgery, or when repeated EEG tests have not provided enough clues about the type of seizure.
Magnetic resonance imaging (MRI) and computed tomography (CT) scans may be used to look at the cause and the location within the brain. The scans can show scar tissue, tumors or structural problems in the brain.
Routine lab tests may be used to rule out other medical conditions that might be causing the seizures.
- A complete blood count (CBC) will provide the doctor with information regarding infection, abnormal electrolyte levels (such as magnesium, potassium and calcium), kidney or liver malfunction or genetic conditions.
- A lumbar puncture (spinal tap) can rule out infections, such as spinal meningitis and encephalitis.
- A toxicology screening can show poisons, illegal drugs or other toxins.
Treatment
For most people with epilepsy, correct treatment can lower or prevent seizures. In some cases, patients may not have any more seizures for the rest of their life.
Partial and generalized seizures are often treated differently. Treatment is based on:
- The type of seizure
- How often seizures happen
- How severe the seizures are
- The patient's age
- The patient's overall health
- The patient's medical history
Anti-seizure (or anti-epileptic) medications can be very helpful. It may take a few tries to get the right drug and right dosage. The doctor will watch for side effects to find the best treatment.
Surgery may be an option if medication can't control the seizures.
A vagus nerve stimulator (VNS) is sometimes implanted and used with anti-epileptic medication to reduce how many seizures a person has. The VNS is a tool placed under the skin of the chest. It sends electrical energy through the vagus nerve in the neck to the brain.
Certain types of epilepsy may be controlled with a ketogenic diet. This is a high-fat, low-carbohydrate diet used most often for children who have not responded to medications.
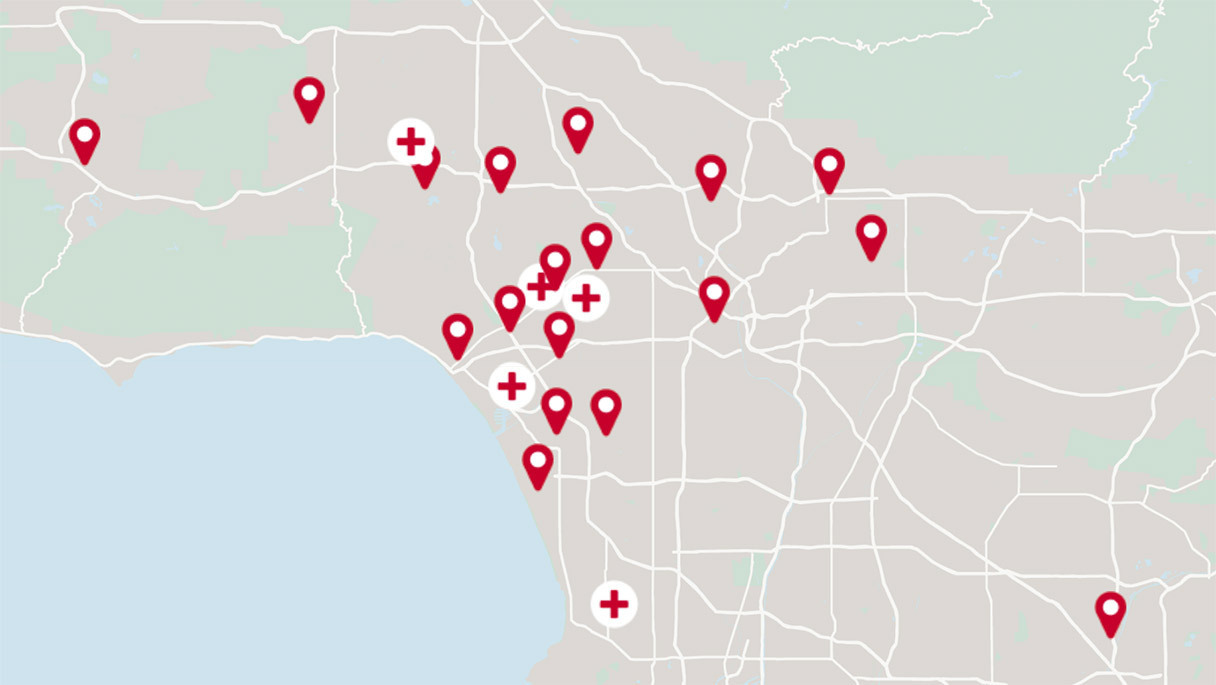
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.