Gastroesophageal Reflux Disease (GERD)/Heartburn
What is GERD?
GERD (gastroesophageal reflux disease) is a digestive disorder. It's caused when gastric acid from your stomach flows back up into your food pipe (esophagus).
Heartburn is the most common symptom of GERD.
What causes GERD?
GERD happens when gastric acid from your stomach backs up into your food pipe (esophagus).
A muscle at the bottom of the esophagus opens to let food from the bottom of the esophagus into the stomach. And it closes to keep food in the stomach. This muscle is called the lower esophageal sphincter (LES). When your LES relaxes too often or for too long, acid backs up into your esophagus. This causes heartburn and may cause damage.
Some lifestyle issues that can cause GERD may include:
- Being overweight
- Overeating
- Eating foods such as citrus, chocolate, and fatty or spicy foods
- Having caffeine
- Having alcohol
- Smoking
- Using aspirin and over-the-counter pain and fever medicines. These include nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen.
Some health problems that may cause heartburn, or make it more likely, may include:
- Swelling of your stomach lining (gastritis)
- Painful sores (ulcers) on the lining of your stomach or esophagus, or the first part of your small intestine (duodenum)
- An allergic condition in the esophagus (eosinophilic esophagitis)
Who is at risk for GERD?
You may be more at risk for GERD if you:
- Have a part of your stomach slide up out of the belly cavity next to your esophagus (hiatal hernia)
- Have a weak lower esophageal sphincter or LES
- Are obese
- Are pregnant
- Use some medicines, such as aspirin or over-the-counter pain and fever medicines such as NSAIDs
- Smoke or are around secondhand smoke
- Drink alcohol
- Are older
What are the symptoms of GERD?
Heartburn, also called acid indigestion, or acid reflux, is the most common symptom of GERD. Heartburn is a burning chest pain that starts behind your breastbone and moves up to your neck and throat. It can last as long as 2 hours. It often feels worse after you eat. Lying down or bending over can also cause heartburn. Another common symptom of GERD is bringing swallowed food up again to the mouth (regurgitation). Some people can have trouble swallowing.
Heartburn is not a GERD symptom for most children younger than 12 years old, and for some adults. They may have a dry cough, asthma symptoms, or trouble swallowing instead.
Each person’s symptoms may vary. GERD symptoms can be caused by other health problems. Always see your healthcare provider to be sure.
How is GERD diagnosed?
To see if you have GERD, your healthcare provider will give you a physical exam and ask about your past health. Some people with typical symptoms may be treated without more testing.
Other tests for GERD may include:
- Upper GI (gastrointestinal) series, also called a barium swallow. This test looks at the organs of the top part of your digestive system. It checks your food pipe (esophagus), stomach, and the first part of your small intestine (duodenum). You will swallow a metallic fluid called barium. Barium coats the organs so that they can be seen on an X-ray.
- Upper endoscopy or EGD (esophagogastroduodenoscopy). This test looks at the lining or inside of your esophagus, stomach, and duodenum. This test uses a thin, lighted tube (endoscope). The tube has a camera at one end. The tube is put into your mouth and throat while you are sedated. Then it goes into your esophagus, stomach, and duodenum. Your healthcare provider can see the inside of these organs. They can also take a small tissue sample (biopsy) if needed.
- Bernstein test. This test helps to see if your symptoms are caused by acid in your esophagus. The test is done by dripping a mild acid through a tube placed in your esophagus to see if that causes the same symptoms. The Bernstein test is rarely done now.
- Esophageal manometry. This test checks the strength of your esophagus muscles. It can see if you have any problems with backward flow of fluid (reflux) or swallowing. A small tube is put into your nostril, then down your throat and into your esophagus. The tube checks how much pressure your esophageal muscles make when they are at rest.
- pH monitoring. This test checks the pH (acid level) in your esophagus. A thin, plastic tube is placed into your nostril, down your throat, and into your esophagus. The tube has a sensor that measures pH level. The other end of the tube outside your body is attached by a wire to a small monitor that records your pH levels for 24 to 48 hours. During this time you can go home and do your normal activities. You will need to keep a diary of any symptoms you feel, and also of the food you eat. Your pH readings are checked and compared to your activity for that time period. Another method is to attach a capsule, about the size of a pencil eraser, to the lining inside the esophagus during an EGD. This sends pH data wirelessly to a receiver that can be worn on your wrist, or some other place. The capsule falls off in about 5 days and passes in your stool.
- Impedance testing. This test is able to see reflux of acid, plus nonacid liquid and air. It can be done with pH monitoring.
How is GERD treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is.
In many cases making diet and lifestyle changes can help reduce GERD symptoms. Always check with your healthcare provider before making any changes.
If you have GERD, be careful about what you eat and drink. Don’t have too much of these:
- Fried and fatty foods
- Peppermint
- Chocolate
- Alcohol
- Citrus fruit and juices
- Tomato products
- Drinks with caffeine, such as coffee, soda, and energy drinks
You should also:
- Eat smaller amounts
- Not overeat
- Quit smoking
- Not drink too much alcohol
- Wait a few hours after eating before you lie down or go to bed
- Lose weight if needed
- Raise the head of your bed 6 inches. (To do this, put bricks, cinderblocks, or bed risers under the bed legs at the head of the bed.) A "wedge" pillow can also be used while sleeping to raise (elevate) your chest and head above the level of your stomach.
Check any medicines you are taking. Some may cause problems with the lining of your stomach or esophagus. You may also want to talk with your healthcare provider about:
- Taking medicines to reduce your stomach acid (antacids)
- Taking medicines called H2-blockers and proton pump inhibitors. Taking these medicines before eating may stop heartburn from happening.
- Taking medicines that help to empty food from your stomach (pro-motility medicines). You will need a prescription for these. But these medicines are rarely used to treat reflux disease unless there are other problems, too.
- Having surgery called fundoplication. This is sometimes done to help keep the esophagus in the right place and to stop the backward flow of fluid (reflux).
What are possible complications of GERD?
If GERD is not treated, it can lead to other health problems. These may include:
- Esophagitis. This is an irritation of the esophagus caused by the acid in your stomach contents.
- Narrowing of the esophagus, also called strictures. This can make it hard to swallow.
- Breathing problems. This happens when stomach contents from your esophagus go into your lungs.
- Barrett’s esophagus. This affects the lining of your esophagus. In some cases it can lead to esophageal cancer.
What can I do to prevent GERD?
Some of the same diet and lifestyle changes that are used to treat GERD can also help to prevent it.
Living with GERD
Your healthcare provider will give you advice on how to manage your GERD symptoms. In most cases you will need to make some diet and lifestyle changes so that GERD pain won’t get in the way of your normal activities.
When should I call my healthcare provider?
Call your healthcare provider if:
- Your GERD symptoms don’t get better with treatment, or they get worse
- You have new symptoms
- You start vomiting
- You have involuntary weight loss
- You have trouble or pain with swallowing
- You have a new cough or trouble breathing
- You have small amounts of blood in your vomit or stool
Call 911
Call 911 or go to the nearest emergency room if any of these occur:
- You have a large amount of blood in your vomit or stool
- You have severe trouble breathing
- You feel weak or faint
Key points about gastroesophageal reflux disease (GERD)
- GERD is a digestive disorder. It is caused by gastric acid flowing from your stomach back up into your food pipe (esophagus).
- Heartburn is the most common symptom of GERD.
- Some lifestyle issues that may cause GERD include being overweight, overeating, having caffeine and alcohol, and eating chocolate and spicy foods.
- There are several tests that can be done to see if you have GERD.
- If it's not treated, GERD can lead to other health problems.
- Making diet and lifestyle changes can help reduce GERD symptoms. Some medicines may also help reduce symptoms.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
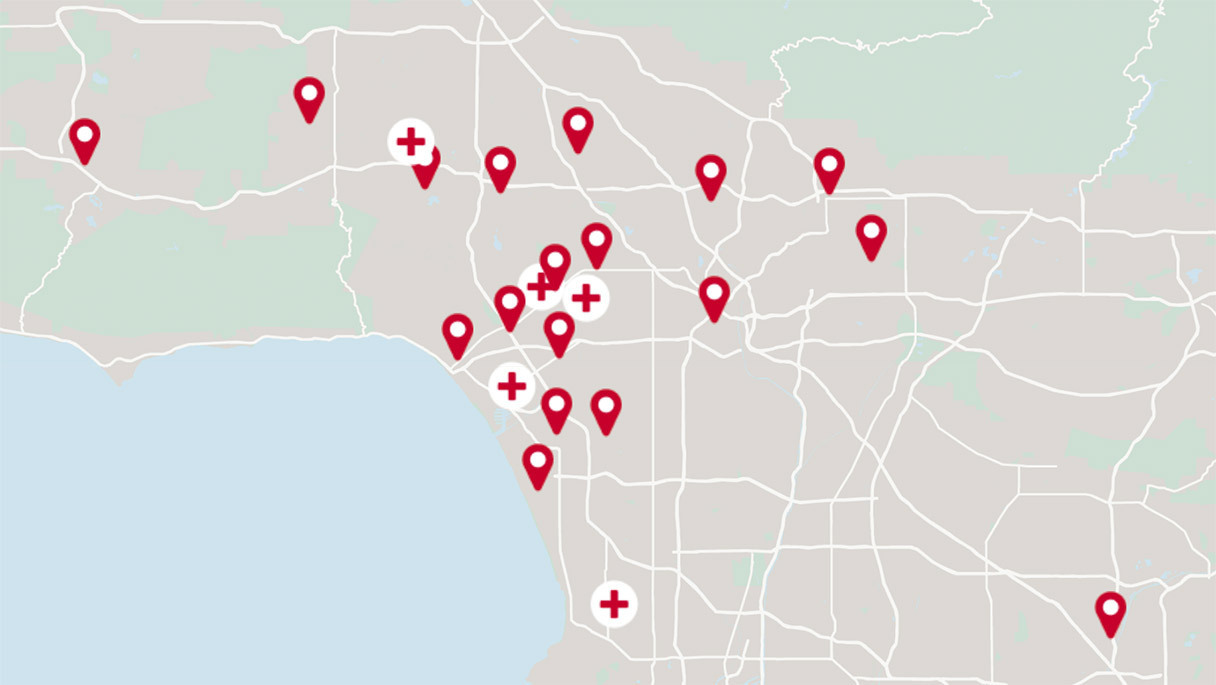
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.