Osteoarthritis
What is osteoarthritis?
Arthritis is a condition that causes pain and inflammation in joints. Osteoarthritis (OA) is the most common type. It's a long-term (chronic), degenerative joint disease. Degenerative means that it gets worse over time. It affects mostly middle-aged and older adults. OA causes the breakdown of joint cartilage. It can occur in any joint. But it most often affects the hands, knees, hips, or spine.
What causes osteoarthritis?
OA can be called primary or secondary. Primary OA has no known cause. Secondary OA is caused by another disease, infection, injury, or deformity. OA starts with the breakdown of cartilage in the joint. As the cartilage wears down, the bone ends may thicken and form bony growths. These growths are called bone spurs. Bone spurs can limit joint movement. Bits of bone and cartilage may float in the joint space. Fluid-filled cysts may form in the bone. These can also limit joint movement.
Who is at risk for osteoarthritis?
The risk factors of OA include:
- Heredity. Some genetic problems may lead to OA. These include slight joint defects or joints that are too loose.
- Extra weight. Being overweight can put stress on such joints as the knees over time.
- Injury or overuse. Severe injury to a joint, such as the knee, can lead to OA. Injury may also result from overuse or misuse over time.
What are the symptoms of osteoarthritis?
The most common symptom of OA is pain after overuse or inactivity of a joint. Symptoms usually happen slowly over years. Symptoms can occur a bit differently in each person. They may include:
- Joint pain
- Joint stiffness, especially after sleep or inactivity
- Less movement in the joint over time
- A grinding feeling in the joint when moved, as the cartilage wears away (in later stages)
The symptoms of OA can be like other health conditions. Make sure to see your healthcare provider for a diagnosis.
How is osteoarthritis diagnosed?
The process starts with a health history and a physical exam. You may also have X-rays. This test uses a small amount of radiation to create images of bone and other body tissues.
How is osteoarthritis treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is. The goal of treatment is to ease joint pain and stiffness, and improve joint movement. Treatment may include:
- Exercise.Regular exercise may help ease pain and other symptoms. This may include stretching and strength exercises.
- Heat treatment. Treating the joint with heat may help ease pain.
- Physical and occupational therapy. These types of therapy may help ease joint pain, improve joint flexibility, and reduce joint strain. You may use splints and other assistive devices.
- Weight maintenance. Keeping a healthy weight, or losing weight if needed, may help to prevent or ease symptoms.
- Medicines.These may include pain relievers and anti-inflammatory medicines. You might take these by mouth as a pill. Or you may rub them on your skin in a cream.
- Injections of a lubricant into the joints.These liquids mimic normal joint fluid.
- Joint surgery. You may need surgery to repair or replace a joint that has severe damage.
Talk with your healthcare providers about the risks, benefits, and possible side effects of all treatments.
What are possible complications of osteoarthritis?
Because OA causes joints to get worse over time, it can cause disability. It can cause pain and movement problems. These can make you less able to do normal daily activities and tasks.
Living with osteoarthritis
Although there is no cure for OA, it's important to help keep joints working. You can ease pain and inflammation. Work on a treatment plan with your healthcare provider. The plan may include medicine and therapy. Work on lifestyle changes that can improve your quality of life. These may include:
- Losing weight. Extra weight puts more stress on weight-bearing joints, such as the hips and knees.
- Exercising.Some exercises may help ease joint pain and stiffness. These include swimming, walking, low-impact aerobic exercise, and range-of-motion exercises. Stretching exercises may also help keep the joints flexible.
- Balancing activity and rest. To reduce stress on your joints, alternate between activity and rest. This can help protect your joints and ease your symptoms.
- Using assistive devices. Canes, crutches, and walkers can help to keep stress off certain joints and improve balance.
- Using adaptive equipment. Reachers and grabbers allow you to extend your reach and reduce straining. Dressing aids can help you get dressed more easily.
- Managing use of medicines. Long-term use of some anti-inflammatory medicines can lead to stomach bleeding. Work with your healthcare provider to create a plan to reduce this risk.
When should I call my healthcare provider?
If your symptoms get worse or you have new symptoms, let your healthcare provider know.
Key points about osteoarthritis
- Osteoarthritis is a chronic joint disease. It affects mostly middle-aged and older adults.
- It starts with the breakdown of joint cartilage.
- Risk factors include heredity, obesity, injury, and overuse.
- Common symptoms include pain, stiffness, and limited movement of joints.
- Treatment may include medicines, exercise, heat, and joint injections. Surgery may be needed to repair or replace a severely damaged joint.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your healthcare provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions.
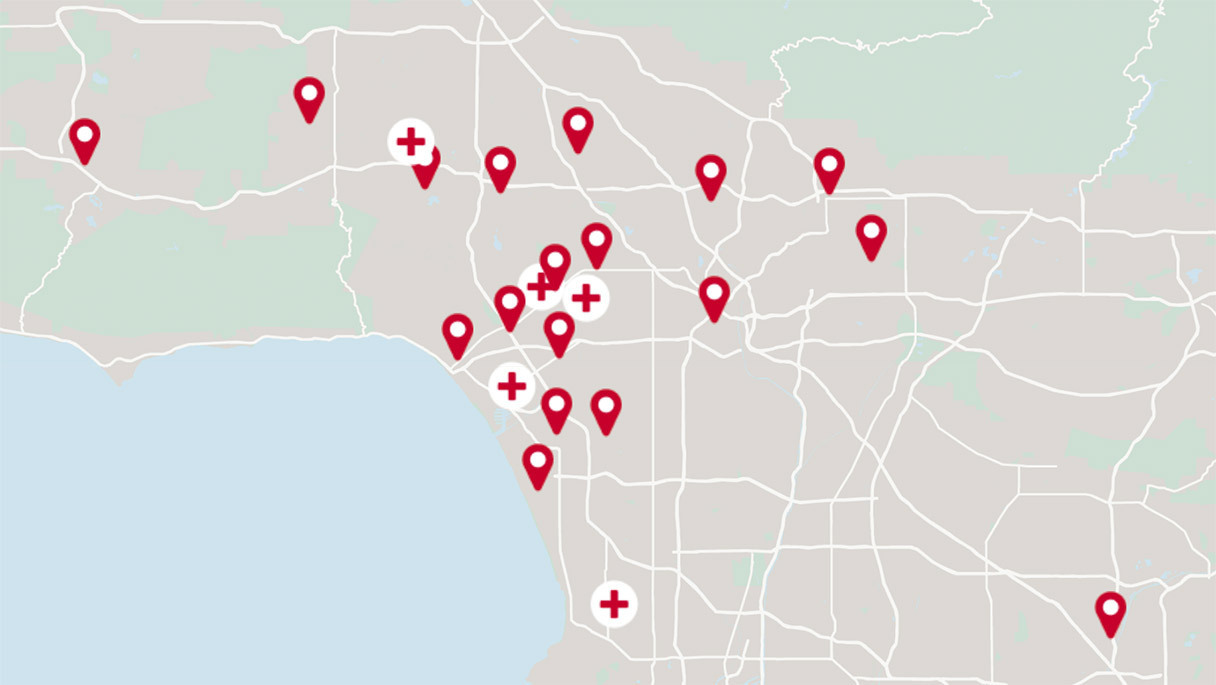
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.