Acute Pancreatitis
What is acute pancreatitis?
Your pancreas is a hardworking organ. It makes enzymes that help you digest food. It also makes insulin to keep your blood sugar levels under control. Pancreatitis is an inflammation of your pancreas. This can be very painful. You may also have nausea, vomiting, and fever. Acute pancreatitis is an emergency that needs care right away. Acute pancreatitis is common and becoming more common.
What causes acute pancreatitis?
Among the many possible causes of acute pancreatitis are:
- Alcohol consumption
- Gallstones
- Genetic abnormalities of the pancreas
- High levels of triglycerides, a type of cholesterol
- Very high levels of calcium
- Infections
- Medicines
- Toxins
- Trauma or injury
Who is at risk for acute pancreatitis?
Anyone can develop acute pancreatitis. But certain people have a higher risk:
- People who have gallbladder disease
- People who drink a lot of alcohol
What are the symptoms of acute pancreatitis?
Symptoms of acute pancreatitis are:
- Fever
- Nausea
- Pain that follows a meal
- Pain that seems to move into other parts of your body, for example, from your upper abdomen to your back, chest, flanks, or lower abdomen
- Pain that may be eased somewhat if you lean forward over your knees
- Severe upper abdominal pain, which may come on slowly or quickly
- Throwing up, but without feeling better afterward
How is acute pancreatitis diagnosed?
To make a diagnosis, your healthcare provider will consider:
- Your overall health and medical history
- Your symptoms, including where the pain is, how intense it is, and when and how it started
- A physical exam
- Lab blood tests. Enzymes from the pancreas are often higher than normal.
- The results of imaging tests such as abdominal CT scan, ultrasound, and MRI
How is acute pancreatitis treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is.
You may need a hospital stay for acute pancreatitis. Treatment may include:
- A procedure to remove a gallstone that’s blocking the bile duct from the pancreas
- Counseling, treatment, and therapy to quit drinking alcohol, if needed
- Limiting food and drink through your mouth to give your pancreas a chance to get better
- Medicines for pain
- Oxygen
- Fluids through a catheter into your vein
- A feeding tube to provide nutrition
- Surgery to take out your gallbladder, if needed
- Surgery, if needed, to remove damaged tissues
What are possible complications of acute pancreatitis?
Complications are problems caused by your condition. They may include:
- Another acute pancreatitis episode
- Development of a pancreatic pseudocyst (a fluid-filled sac)
- Infections
- Kidney failure
- Lung failure
- Shock
- Chronic (long-term) pancreatitis
- Death from multiple organs failing
Can acute pancreatitis be prevented?
Depending on the cause of your acute pancreatitis, your healthcare provider might recommend these steps to help you prevent another event:
- Not drinking alcohol at all
- Making lifestyle changes or taking medicine to lower your triglyceride level
- Removing your gallbladder if a gallstone caused your condition
Living with acute pancreatitis
Follow your healthcare provider’s recommendations for taking care of yourself after you’ve had acute pancreatitis. This might mean:
- Not drinking alcohol
- Stopping smoking
- Eating differently
- Reducing triglycerides through diet, exercise, weight loss, and medicines
- Getting your blood sugar levels tested regularly
- Having more surgery or treatment to reduce your risk
When should I call my healthcare provider?
Seek care right away if you have the symptoms of acute pancreatitis, especially severe abdominal pain, vomiting, and fever.
Key points about acute pancreatitis
- Acute pancreatitis is a medical emergency.
- Gallstones, alcohol consumption, certain medicines, injury, infection, and genetic problems can cause acute pancreatitis.
- Symptoms include upper abdominal pain, pain after eating, nausea, and fever.
- You may need to be hospitalized to treat acute pancreatitis.
- Treatment includes oxygen, medicines, and possibly surgery.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your healthcare provider tells you.
- At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your healthcare provider gives you.
- Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions.
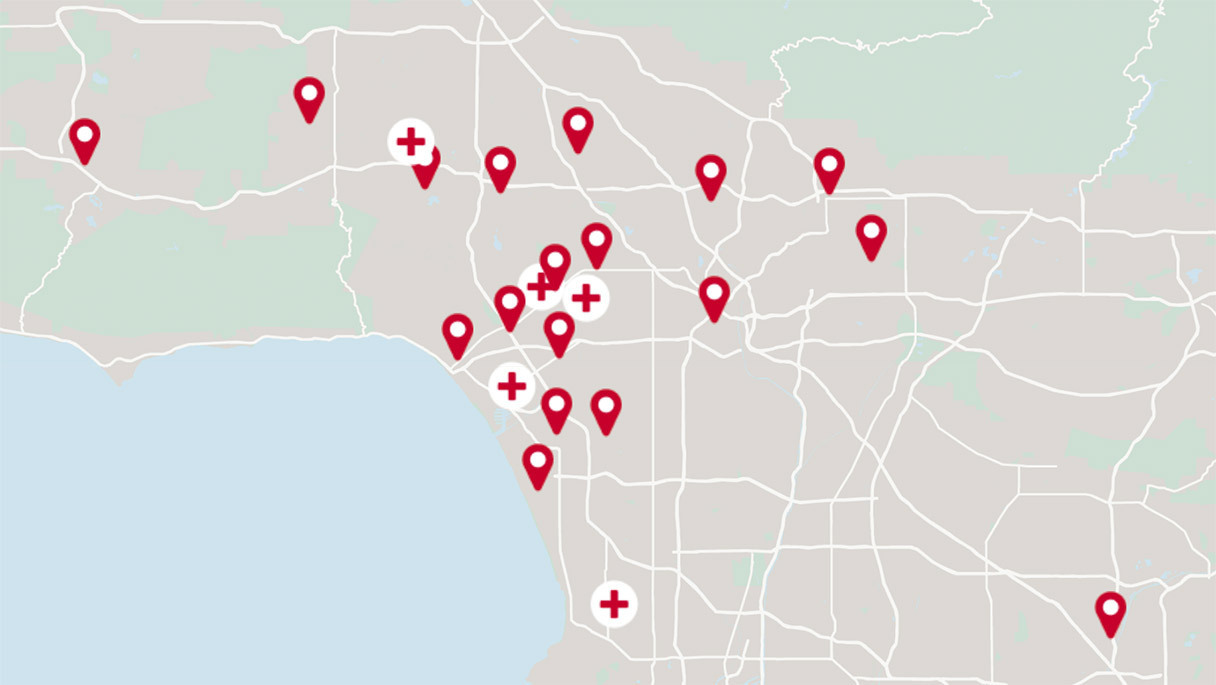
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.