Spinal Compression Fractures
Overview
A compression fracture is usually defined as a vertebral bone in the spine that has decreased at least 15 percent to 20 percent in height due to fracture.
There are three types of compression fractures:
Wedge fracture — This fracture usually occurs in the front of the vertebra, collapsing the bone in the front of the spine and leaving the back of the same bone unchanged, which results in the vertebra taking on a wedge shape.
Crush fracture — If the entire bone breaks, rather than just the front of the vertebra, it may be called a crush fracture.
Burst fracture — This type of fracture involves some loss of height in both the front and back walls of the vertebral body (rather than just the front of the vertebra). Making this distinction is important because burst fractures can be unstable and can result in progressive deformity or neurologic compromise.
Symptoms
Vertebral fractures are usually followed by acute back pain and may lead to chronic pain, deformity (thoracic kyphosis, commonly referred to as a dowager's hump), loss of height, crowding of internal organs, and loss of muscle and aerobic conditioning due to lack of activity and exercise.
The main clinical symptoms of vertebral fractures typically include one or a combination of the following:
- Sudden onset of back pain
- Worse pain while standing or walking
- Less intense pain while lying on one's back
- Limited spinal mobility
- Height loss
- Deformity and disability
Because the majority of damage is limited to the front of the vertebral column, the fracture is usually stable and rarely associated with any nerve or spinal cord damage.
A common problem with a vertebral fracture is that it is not recognized or accurately diagnosed. Instead, the patient's pain is often just thought of as general back pain — such as from a muscle strain or other soft-tissue injury — or as a common part of aging. As a result, about two-thirds of the vertebral fractures that occur each year are not diagnosed and therefore are not treated.
Causes and Risk Factors
Osteoporosis is by far the most common cause of vertebral compression fractures, especially in women over age 50. It is more common than most people think in people between the ages of 40 and 50, and it is reasonably common in men over age 50.
Osteoporosis causes bones to thin and become brittle and weak. The thinning bones can collapse during normal activity, leading to a spinal fracture. These compression fractures can cause a great deal of pain and can permanently alter the shape and strength of the spine.
Spinal fractures due to osteoporosis often occur while a person is doing something that causes relatively minor trauma to the spine, such as opening a window, suffering an insignificant fall or twisting while lifting.
Advanced cases of osteoporosis can lead to a vertebral fracture being caused by routine activities that normally would not cause trauma, such as sneezing, coughing or turning over in bed.
Trauma to the spinal vertebrae also can lead to minor or severe fractures. Such trauma could come from a fall, a forceful jump, a car accident or any event that stresses the bones in the spine past its breaking point.
Tumors also can weaken the spinal vertebrae to the point where they may fracture. It is not uncommon for metastatic cancer that starts in another part of the body to spread to bones in the spine.
A compression fracture of the spine that appears for little or no reason may be the first indication that an unrecognized cancer has spread to the spine. Cancer or multiple myeloma should be considered in patients who also have hypercalcemia, otherwise unexplained anemia, weight loss or proteinuria.
Diagnosis
The diagnostic process includes a complete history of the patient's condition, medical history and family history.
After taking the patient's history, the physician will do a physical examination in an effort to determine the cause of the pain and rule out other possible problems.
If a vertebral compression fracture is suspected, the doctor will test for tenderness and sensitivity near specific vertebrae along the spine. Based on the patient's history and physical exam, if a vertebral fracture is suspected, an X-ray will be ordered to confirm the diagnosis.
Depending on the physician's findings from the patient's history, physical exam and X-ray, additional diagnostic tests may also be needed, such as:
A CT scan — To see whether the fractured bone is stable and if nerves near the fracture are being irritated or affected by the fracture.
An MRI — May be ordered if the doctor suspects another cause of the patient’s pain, or if there is a chance that nerves near the fracture are affected. An MRI can also tell if the fracture is old or new.
A nuclear bone scan — May be used to help determine when the fracture occurred. The age of the fracture is sometimes important to know to help guide treatment options.
Treatment
Conservative management is the traditional first-line therapy for painful vertebral compression fractures. These treatments include:
- Bracing
- Physical therapy
- Nonsteroidal anti-inflammatory medications
Surgical management is recommended for a patient who has not clinically improved despite adequate conservative care.
The two minimally invasive surgical procedures for osteoporotic compression fractures are kyphoplasty and vertebroplasty.
Spinal fusion may be recommended if the fracture is considered unstable with neurologic injury, angulation of the spine is greater than 20 degrees, there is subluxation or dislocation of the spine, or there is greater than a 50 percent spinal canal compromise.
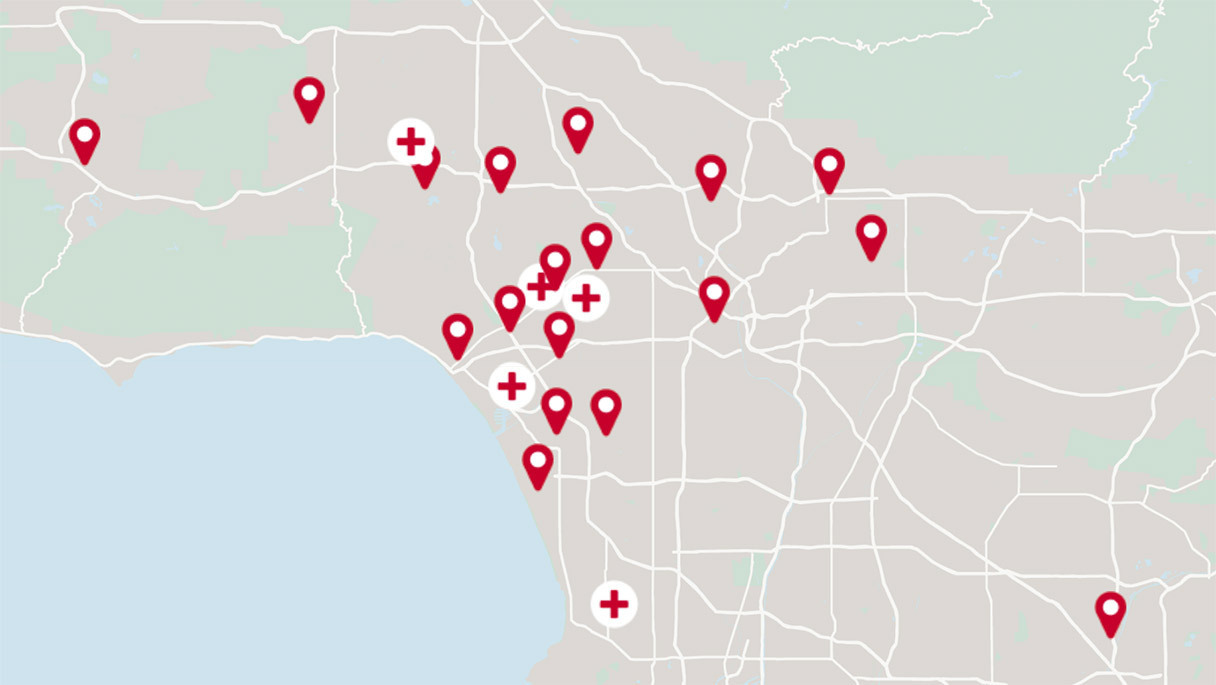
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.