Tracheomalacia
Overview
Tracheomalacia is a rare condition that happens when the cartilage of the windpipe, or trachea, is soft, weak and floppy. This can cause the tracheal wall to collapse and block the airway, making it hard to breathe.
There are two types of tracheomalacia:
Congenital — this is present from birth and may be associated with abnormalities in the trachea.
Acquired — this develops after birth and can be caused by trauma to the trachea, chronic tracheal infections, intubation that lasts too long or polychondritis (inflammation of the cartilage in the trachea).
Symptoms
Tracheomalacia can have no symptoms, especially if the condition is very mild.
However, the more the airway is blocked, the more severe the symptoms are. Symptoms of tracheomalacia are often attributed to other conditions, such as emphysema or asthma.
The major symptoms in adults are:
- Difficulty breathing
- High-pitched or rattling, noisy breaths
- Noisy breathing, that may change when body position shifts and may improve during sleep
- Severe coughing fits that may interrupt daily activities
- Episodes of feeling as though you are choking
- Wheezing
- Lightheadedness due to coughing fits
- Recurrent pulmonary infections
Causes and Risk Factors
Some causes of tracheomalacia are prolonged intubation (as when a patient is under general anesthesia for a long time with a tube in their throat to help them breathe), a history of tracheotomy, chronic bronchitis , emphysema , or diffuse pulmonary fibrosis.
Diagnosis
Diagnosis of tracheomalacia usually begins with a physical exam and a review of the patient’s medical history and symptoms.
Diagnostic tests such as a chest x-ray, blood tests, or other procedures are used to diagnose any infection or other related conditions that may be present.
Other tests such as a bronchoscopy may be used to look at the tissue within the chest wall or at the airway to examine inflammation or other signs of infection.
Treatment
If caused by infection, tracheomalacia is treated by addressing the infection that is causing the symptoms. Antibiotic medications to help fight the infection and reduce inflammation are often prescribed.
Prescription narcotics such as Vicodin may be provided to help reduce severe pain. Other prescription medications that can help control pain include antidepressants and anti-seizure drugs.
In-office or at home physical therapy exercises may also be prescribed as treatment. Stretching exercises that focus on the chest muscles can help with pain and tightness related to inflammation.
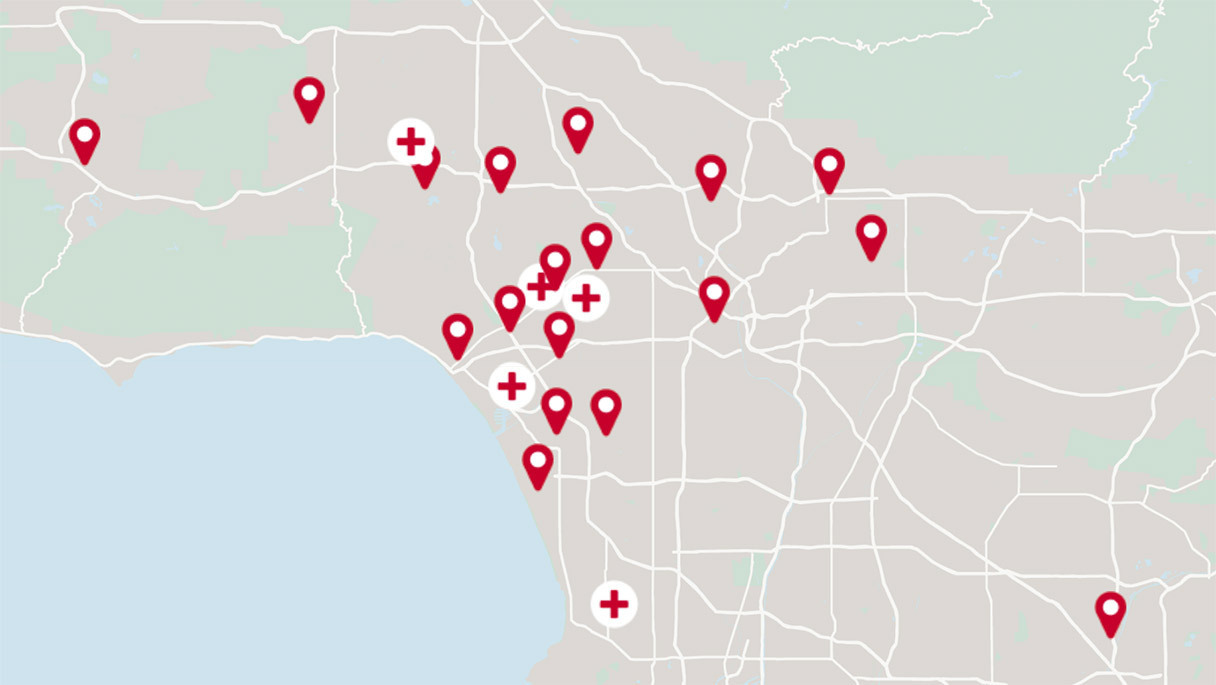
The multidisciplinary team at the Advanced Lung Disease Program can determine the best treatment option for each patient.
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.