Ventricular Tachycardia (VT)
What is ventricular tachycardia (VT)?
Ventricular tachycardia (VT) is a fast, abnormal heart rhythm (arrhythmia). It starts in your heart’s lower chambers, called the ventricles. VT is defined as 3 or more heartbeats in a row, at a rate of more than 100 beats a minute. If VT lasts for more than a few seconds at a time, it can become life-threatening. Sustained VT is when the arrhythmia lasts for more than 30 seconds. Or when it's linked to a blood flow issue, such as abnormal blood pressure. Otherwise the VT is called nonsustained. The rapid heartbeat doesn't give your heart enough time to fill with blood before it contracts again. This can affect blood flow to the rest of your body.
What causes VT?
VT is produced by 2 mechanisms:
- Reentry. This is an abnormal heart circuit within the ventricular muscle that is set in motion or triggered.
- Automaticity. Abnormal ventricular muscle that becomes self-activated.
Who is at risk for VT?
VT is often linked to other heart problems that can damage or change normal heart muscle function. Damaged heart muscles can create abnormal electrical circuits that result in VT. You may be more at risk for VT if you have:
- Abnormal heart valves
- Cardiomyopathy
- Heart failure
- Coronary artery disease
- Heart attack
Some types of genetic diseases can also lead to VT. These include:
- Conditions that make it hard for the heart to pump blood, such as hypertrophic cardiomyopathy
- Diseases that can develop inside the heart muscle, such as sarcoidosis (caused by inflammation)
- Diseases that change the electric properties and heart rhythm itself (such as Brugada syndrome or catecholaminergic polymorphic VT)
In some cases, VT occurs when there are no other heart problems. This may be seen in self-activating VT.
What are the symptoms of VT?
When you have VT, your heart beats very fast. This may only last for a few seconds. Longer episodes may be dangerous. The heart beats so fast that it can’t get enough blood to the rest of your body.
Symptoms of VT may include:
- Fast heartbeat or a fluttering feeling in the chest (palpitations)
- Dizziness
- Lightheadedness
- Chest pain
- Neck tightness
- Shortness of breath
- Fainting
- Cardiac arrest
In some cases, there are no symptoms at all.
How is VT diagnosed?
To diagnose VT, recording of the heart rhythm is needed. You may need an electrocardiogram (ECG). This test records your heart rate and rhythm. Your provider may want to closely watch your heart’s activity for a longer time using a Holter monitor or event recorder. VT may be diagnosed in the hospital with continuous heart monitoring called telemetry. It may also be seen and diagnosed during a stress test. Some smartphones along with a handheld recording device may also be used to record VT when you're having symptoms.
In some cases, your provider may think you have VT, but hasn’t been able to document it. Implantable loop recorders may then be used to record the heart rhythm for up to 3 years. These are small electronic recording devices that are about the size of a pinky finger. They're injected into the skin overlying the heart.
How is VT treated?
Treatment will depend on your symptoms. No treatment may be needed if:
- You don’t have underlying heart disease
- You're not having difficult symptoms
- Your VT episodes don’t last a long time
If you do have symptoms, your healthcare provider might prescribe medicine (a beta-blocker, calcium channel blocker, or antiarrhythmic medicine) to control your heart rhythm.
For VT that's sustained or life-threatening, a small device called an ICD (implantable cardiac defibrillator) may be used. This is especially true when there's no reversible cause found. Or if you have another condition that makes you more likely to have more episodes of VT. The ICD is implanted into your chest. It's connected to your heart with wires. When an abnormal heartbeat occurs, the ICD can overdrive pace the VT to stop it. Or if needed, the ICD can send an electric shock to restore your normal heartbeat. Newer ICDs can be implanted just below the left armpit. This is done using a wire that's tunneled over the sternum instead of inside the heart.
Some VT may be treated with catheter ablation. This procedure uses radiofrequency energy to destroy the abnormal heart tissue that's causing the rapid heartbeat.
What are possible complications of VT?
Some people may have mild symptoms from VT, or no symptoms at all. But for others, VT can be very dangerous. It can lead to fainting (syncope), sudden cardiac arrest, and death.
Can VT be prevented?
VT prevention focuses on treating the underlying heart problems that cause the disorder. This may include:
- Taking medicines for heart failure
- Treating heart artery disease
- Having surgery to fix heart valve problems
- Following a heart-healthy diet and exercise plan, to help reduce your risk for some of these conditions
For some people, caffeine or alcohol can be a trigger for VT episodes. Don't take these things if they affect your VT.
Living with VT
If your healthcare provider diagnoses VT, follow their treatment plan closely. Take all medicines as prescribed and tell your provider about any medicines you may be taking for other health problems. Discuss your alcohol, tobacco, or caffeine use with your healthcare team.
When should I call my healthcare provider?
If you have any of these symptoms, call 911 :
- Chest pain or pressure
- Shortness of breath
- Lightheadedness
- Dizziness
- Fainting
- Persistent rapid heartbeat
Key points about VT
- Ventricular tachycardia (VT) is a fast, abnormal heart rhythm. This may last for only a few seconds or for a longer time.
- VT that lasts for only a few seconds may not need to be treated.
- Longer episodes of VT may be dangerous and require treatment and prevention.
- Some diseases that result in heart muscle damage can lead to VT.
- Treatment may include medicines, ablation therapy, or an implantable device to check and correct your heartbeat.
- Call 911if you feel lightheaded or dizzy, or have chest pain or a sustained rapid heartbeat.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
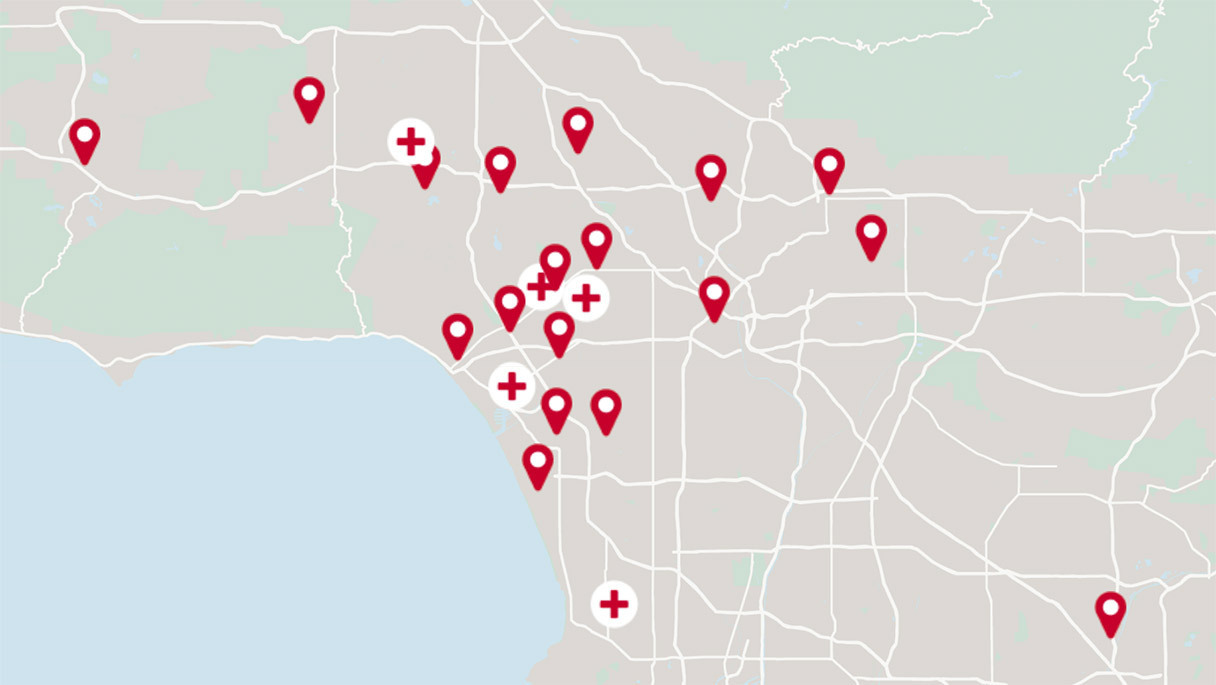
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.