Find a Doctor
With 3,000+ providers available, we’ve got the perfect fit for you.
With 3,000+ providers, we can help find care for you.
Overall patient satisfaction score based on more than %token% ratings
Looks like we do not have any matches for
Check your search for typos or try a different word or phrase.
This provider practices at Guerin Children’s. Learn more
Looks like we do not have any matches for your search.
Check your search for typos or try a different word or phrase.
Filters
Filter Results
Compare Providers
Add another provider to compare
Search for a specific doctor above or choose the type of care you need below:
24/7 Virtual Care
Chat with a provider in English or Spanish through Cedars-Sinai Connect for ages 3+.
Primary Care
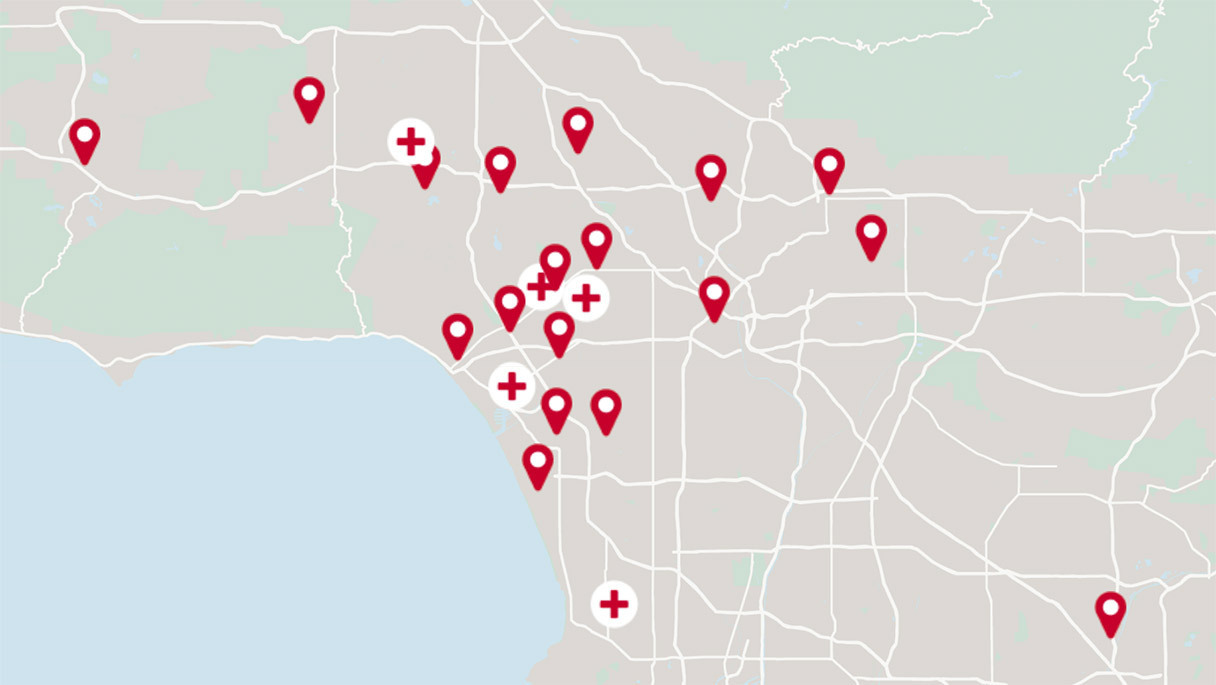
Offering online scheduling, virtual care options and more than 30 locations.
Urgent Care
Walk-in locations open 7 days a week.
Get your flu shot today
Learn the latest vaccine information and schedule your appointment.