Secondary-Progressive Multiple Sclerosis
Overview
Multiple Sclerosis (MS) is a disease of the central nervous system (CNS), which is made up of the brain, spinal cord and optic nerve. This disorder causes destruction of the coating (myelin) that surrounds and protects nerve fibers (axons). As a result, the damage disrupts the normal flow of messages (nerve impulses) from the CNS, causing a reduction or loss of body function. In many cases, the nerve fibers (axons) are also destroyed.
Secondary-progressive multiple sclerosis (SPMS) is the form of the disease that develops from relapsing-remitting multiple sclerosis (RRMS) . The MS disease course varies across individuals and not all patients who have RRMS will develop SPMS. Currently it is not possible to predict who will eventually develop SPMS, but individuals who have frequent severe relapses and large numbers of brain and spinal cord at the time of diagnosis seem to be at higher risk. There is some evidence that the use of effective medications during the RRMS phase of the disease can slow down or possibly prevent the transition to SPMS.
Patients with SPMS generally have fewer relapses than they would with RRMS, because the inflammation has decreased. However, because nerves have begun to be damaged or lost at this stage of the condition, a worsening of the condition is generally experienced.
Symptoms
Symptoms of SPMS are similar to those of primary-progressive multiple sclerosis (PPMS). The main symptom of both forms of the condition is gradual worsening of disability.
This may be experienced through increased:
- Fatigue
- Numbness or tingling
- Vision problems, such as double vision
- Spasticity or stiffness of the muscles
- Bowel and bladder problems, such as urgent need to urinate
- Problems with cognition, such as learning and memory or information processing
- Difficulty with walking and coordination
Patients with SPMS may experience relapses and remission of symptoms, but the remissions aren’t complete and symptoms often remain present during these times.
Causes and Risk Factors
SPMS can only be diagnosed in patients who have had RRMS, but the cause of SPMS is unknown.
Since the risk of multiple sclerosis is significantly higher when a parent has been diagnosed with the disease, genetic factors may play a role. The unusual relationship between a person's geographic location during childhood and the risk of multiple sclerosis later in life suggests there may be environmental factors at work in the disease.
SPMS affects women twice as often as men and is more common in Caucasian patients.
Diagnosis
Diagnosis of SPMS begins with a detailed medical history and neurological examination. Since multiple sclerosis can have symptoms similar to those of other nervous system disorders, diagnostic tests help rule out other causes and confirm a diagnosis. These tests may include a magnetic resonance imaging (MRI) scan of the brain and spinal cord. More than 90 percent of people who have multiple sclerosis have an abnormal MRI. For people already diagnosed with multiple sclerosis, MRI scans also may be used to follow the progression of the disease.
The patient's medical team may order a lumbar puncture, also known as a spinal tap, and cerebrospinal fluid analysis, as well as nerve function tests. Blood tests may be performed to rule out other conditions that have similar symptoms.
There is no single diagnostic procedure to confirm SPMS. Generally, after a diagnosis of RRMS has been established, the physician will observe the patient's symptoms over a period of time in order to determine if they are associated with SPMS.
Treatment
There is no cure for secondary-progressive multiple sclerosis. If a patient has SPMS with relapse episodes, corticosteroids can be given to shorten and lessen the severity of the relapse. Symptoms of SPMS can affect a patient's daily life and physical and occupational therapy may be used to manage symptoms and adjust patients to living and working situations.
Certain medications may be used to reduce the frequency and severity of relapse episodes a patient experiences. Interferon beta medications have been approved by the FDA to treat relapsing-remitting forms of multiple sclerosis, including SPMS if relapses are present. These medications are injected into the muscle and aid in reducing inflammation.
Other medications may address specific symptoms such as:
- Depression
- Muscle spasms
- Need for frequent urination
- Erectile dysfunction
Choosing the right medication requires careful consideration of the risks and benefits, along with close collaboration with an experienced neurologist with experience in treating the disease, such as those at the Multiple Sclerosis Center in Cedars-Sinai's Department of Neurology.
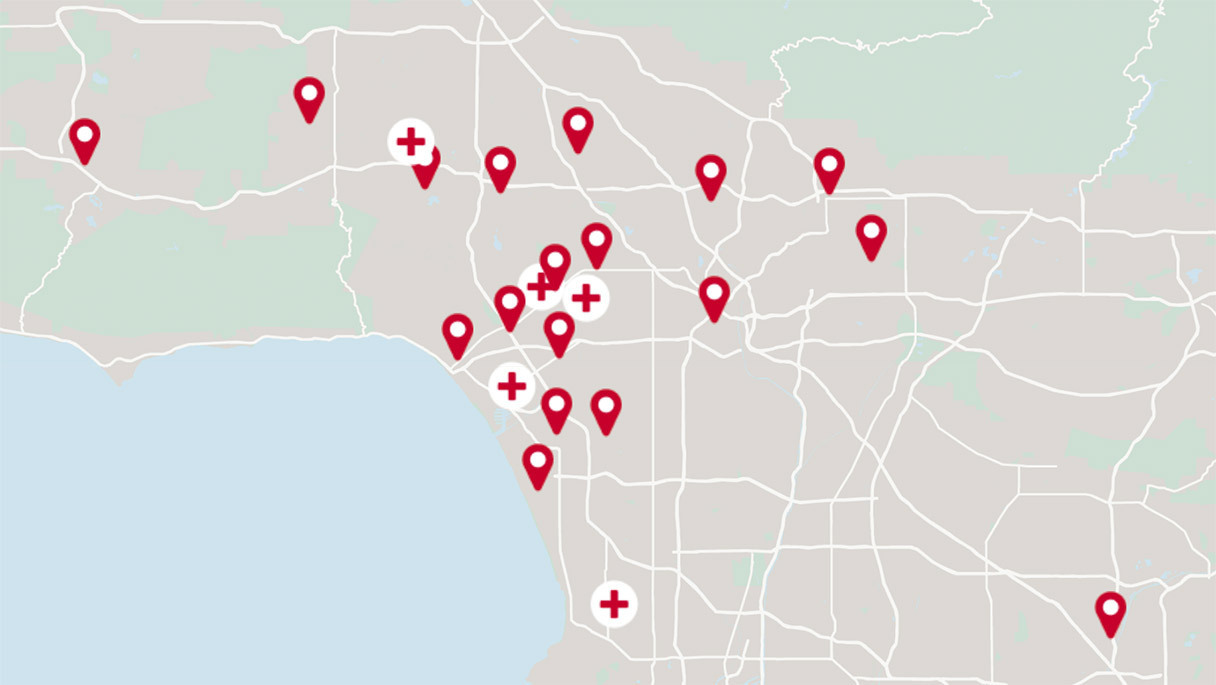
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.