Vulvovaginal Infections
Infections of the vagina and outer female genitals include conditions caused by bacteria, viruses, cancer, non-cancerous tumors and tissue growths, foreign bodies or fistulas (abnormal passages between organs or an organ and a body cavity that allow fluids to pass from one to the other). These infections include:
- Bacterial vaginosis, which represents about 60% of all vaginal infections.
- Yeast infections, which account for 30 to 35 percent of vaginal infections. Most are due to Candida albicans. Yeast appears in 15 to 20 percent of nonpregnant and 20 to 40 percent of pregnant women.
- Trichomonas vaginitis (swelling, redness and tenderness of the vagina caused by trichomonas), which is a sexually transmitted disease. It is responsible for between five and 10% of vaginal infections.
- Herpes simplex virus (HSV), which causes genital ulcers (sores). It is different from syphilis and chancroid.
- Human papillomavirus genital warts, which are the most common viral sexually transmitted disease. About six percent of women between the ages of 20 and 34 have this infection.
Symptoms
Vulvovaginal infections affect primarily the moist walls of the vagina and, to a lesser degree the vulva. Specific symptoms differ with the cause of the condition. For example:
- Yeast infections cause itching and a white discharge that looks like cottage cheese.
- Trichomonas vaginitis exhibits no symptoms at all for about half the women who have the organism. The other half may experience a heavy vaginal discharge (frothy, yellowish green and alkaline) with a fishy odor. Other symptoms include pain when emptying the bladder (urinating) and when having sex. The walls of the vagina may be swollen and, in serious cases, strawberry colored.
- Herpes simplex virus (HSV) has a five-to seven-day growing period before symptoms appear. This makes it easy to spread between sexual partners. When a woman first is infected, her symptoms may include feeling unwell, swollen lymph nodes in the groin and a fever that usually goes away in a week. Painful ulcers develop on the genitals and heal in about 21 days. The virus comes back from time to time. When it returns, a sense of numbness or tingling may be felt where the ulcer is developing. Recurrences tend to be milder and in one place. Ulcers heal in about 10 days. A person can infect others for about four days after the symptoms have gone away.
- A watery discharge, especially if bloody, may indicate a malignancy. Other causes of bleeding include cervical polyps and vaginal atropy, shrinking or wasting of the vagina walls. These usually happen after menopause.
- Bacterial vaginosis causes a fishy smelling discharge. Itching and irritation are also common.
Causes and Risk Factors
Vaginal infections have a variety of causes, and risk factors vary with the specific cause of the infection. For example:
- Using an intrauterine device may put a woman at greater risk of getting bacterial vaginosis or a yeast infection.
- Having multiple sex partners or having sex with a person who has certain bacteria, viruses or other organisms adds to the risk of vaginal problems, including bacterial vaginosis, herpes simplex, trichomonas vaginitis or genital warts.
- Women who are pregnant, diabetic, have recently used an antibiotic, regularly use corticosteroids, have AIDS or who have weakened immune systems are at greater risk of getting a yeast infection.
Diagnosis
Bacterial vaginosis. Diagnosis is made during a pelvic examination. The doctor will check for signs of a discharge and a fishy smell. The doctor may measure the level of acidity in the vaginal area and take samples to examine under the microscope.
Candidal vaginitis. Diagnosis is made through a pelvic exam and by measuring how acidic or alkaline the vagina is. The doctor will also check for yeast cells under the microscope.
Trichomonas vaginitis. A pelvic exam will show inflamed areas in the cervix and vagina that have a strawberry appearance. Cells may also be taken so they can be examined under the microscope.
Treatment
The type of treatment given depends on the cause of the condition. In some cases, treatment completely cures the condition. In others, it relieves symptoms and shortens the period of time the person is affected. For example, herpes simplex cannot currently be cured, but timely anti-viral drugs can help reduce its effect. Other treatments for vulvovaginal infections may include:
- Vaginal creams
- Treatment of a woman's sexual partner in certain types of conditions
- Genital warts may be treated by applying an acid solution. Other treatments are freezing, burning or using laser therapy on the warts
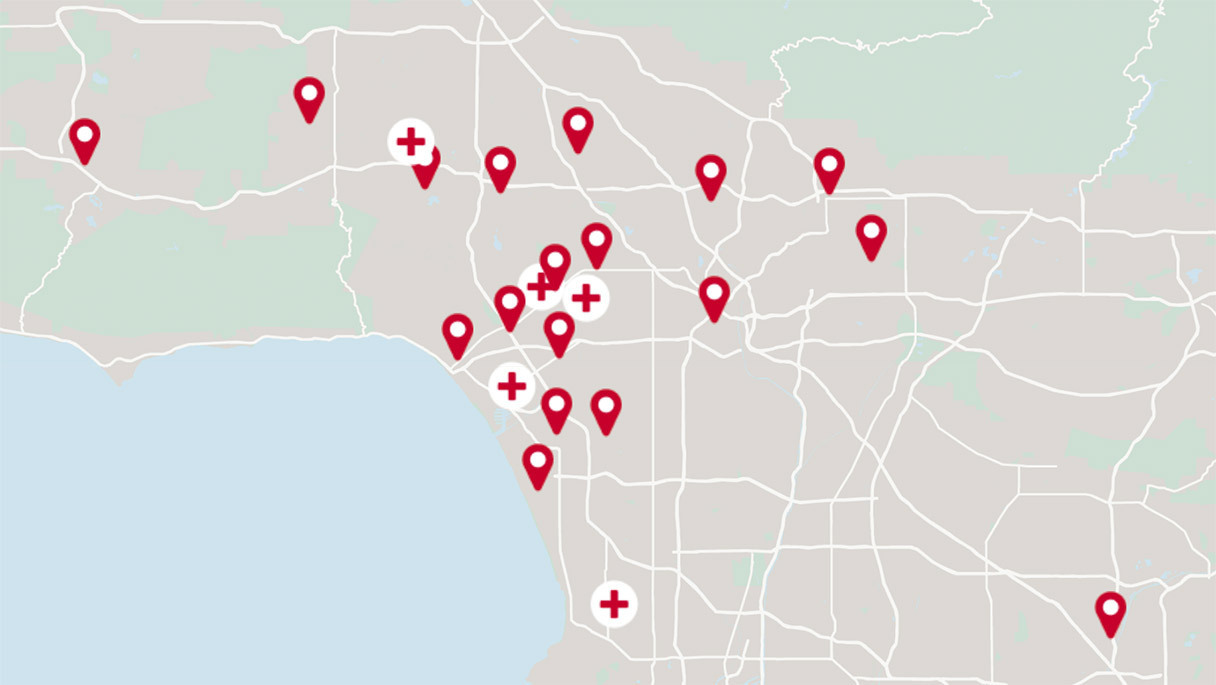
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.