Palate Cancer
What is cancer of the palate?
The palate is commonly called the roof of the mouth. It is divided into two parts: the bony hard palate in the front, and the fleshy soft palate (called the velum) in the back of the mouth. The hard palate is part of the oral cavity and the soft palate is part of the oropharynx.
The hard palate creates a barrier between the mouth and the nasal cavity. A natural opening in the palate for nerves and blood vessels (near the third molar) can create a passageway for a tumor to spread into the nasal cavity.
The soft palate closes the nasal passage during swallowing so food does not enter the nose. It also helps create speech sounds. If the palate does not function correctly during speech, air escapes through the nose, and the speech has a nasal sound. During a sneeze, the soft palate closes the nasal passage to protect it. Substances in the sneeze are thrown out into mouth.
What are the causes and risk factors for cancer of the palate?
Tobacco and alcohol use are risk factors for cancer of the soft palate.
Reverse smoking is a risk factor for cancer of the hard palate. In reverse smoking, the lit end of the cigarette is placed in the mouth. Intense heat is generated during this style of smoking.
What are symptoms of cancer of the palate?
Most cancer of the palate is squamous cell. Cancer of the palate usually is noticed first as an ulcer in the mouth. At first the ulcer is painless, but it later becomes painful. Other symptoms:
- As the mass grows it can bleed.
- A foul odor in the mouth.
- Loose teeth or dentures no longer fit.
- Changes in speech.
- Difficulty swallowing.
- Inability to open the jaw (trismus).
- A lump in the neck.
How is cancer of the palate diagnosed?
The surgeon will examine the palate with a mirror or a small, flexible scope. A tissue sample (biopsy) may be taken of any abnormal areas. A pathologist will then examine the sample under a microscope.
If palate cancer is diagnosed early, the treatment is very successful. The doctor may order the following imaging procedures if it is suspected that the cancer has spread beyond the palate:
- Blood tests
- X-rays or CT scan to determine if the tumor has spread to the lung
- Fine needle aspiration biopsy. A thin needle is placed into the mouth. The cells are suctioned into a syringe and then examined under a microscope to determine if the lump is cancerous.
- Imaging studies to determine if the tumor has invaded nearby tissues or other organs in the body.
- Orthopantomography (Panorex) is a panoramic X-ray of the upper and lower jaw. It shows a view from ear to ear and it helps determine if a tumor has grown into the jaw bone.
- CT scan. A special type of X-ray that makes a series of detailed pictures, with different angles, of areas inside the mouth and neck. A computer is linked to the X-ray machine. A dye may be injected into a vein or swallowed in a pill to help highlight the organs or tissues on the X-ray. This procedure is also called computed tomography, computerized tomography and computerized axial tomography.
- MRI (magnetic resonance imaging). A machine uses a magnet, radio waves and a computer to make detailed pictures of areas inside the mouth and neck. This procedure is also called nuclear magnetic resonance imaging.
- PET scan. During a positron emission tomography scan (PET), a small amount of radioactive glucose (sugar) is injected into a vein. The scanner makes computerized pictures of the areas inside the body. Cancer cells absorb more radioactive glucose than normal cells, so the tumor is highlighted on the pictures.
How is cancer of the palate treated?
Radiation Therapy
Radiation therapy, including intensity modulated radiation therapy, stops cancer cells from dividing and slows the growth of the tumor. Radiotherapy also destroys cancer cells and can shrink or eliminate tumors. Intensity modulated radiation therapy allows the use of more effective radiation doses with fewer side effects than conventional radiotherapy techniques.
Radiation therapy involves five to six weeks of daily treatments.
Chemotherapy
Chemotherapy is prescribed for different reasons:
- Together with radiotherapy as an alternative to surgery (called chemoradiation)
- After surgery to decrease the risk of the cancer returning
- To slow the growth of a tumor and control symptoms when the cancer cannot be cured (palliative treatment)
Chemoradiation
This is a combination of radiation therapy and chemotherapy.
Radiation therapy used alone or with chemotherapy is the primary treatment for moderate or advanced cancers in order to preserve the soft palate and its function.
Radiotherapy can be combined with chemotherapy and surgery.
Treatments for Cancer of the Soft Palate
Laser microsurgery is used for small and medium-sized tumors in the soft palate. The surgeon looks at the soft palate, through the mouth and nose, using a special instrument. After the surgeon locates the tumor, a laser is used to divide the tumor into sections. The sections are then removed and a pathologist examines the cells for cancer.
Transoral laser microsurgery can preserve normal tissues, causes less pain, and can help maintain speech and swallowing.
Treatments for Cancer of the Hard Palate
Surgery is the preferred treatment for cancer of the hard palate. The bone closest to the tumor often contains cancer cells and part of it may also need to be removed. If the tumor is small, the excised area can be closed after surgery.
If the tumor is large, the excised area cannot be closed and a prosthetic device is needed to cover the opening in the roof of the mouth. The prosthesis looks similar to a denture plate.
If the lymph nodes in the neck are affected, the nodes may need to be removed.
Key points
- The palate is divided into two parts: the bony hard palate in the front, and the fleshy soft palate (called the velum) in the back of the mouth.
- Cancer of the palate usually first noticed as an ulcer in the mouth. At first the ulcer is painless, but later becomes painful.
- Tobacco and alcohol use are risk factors for cancer of the soft palate.
- Cancer of the palate can be treated with surgery, radiation and chemotherapy.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
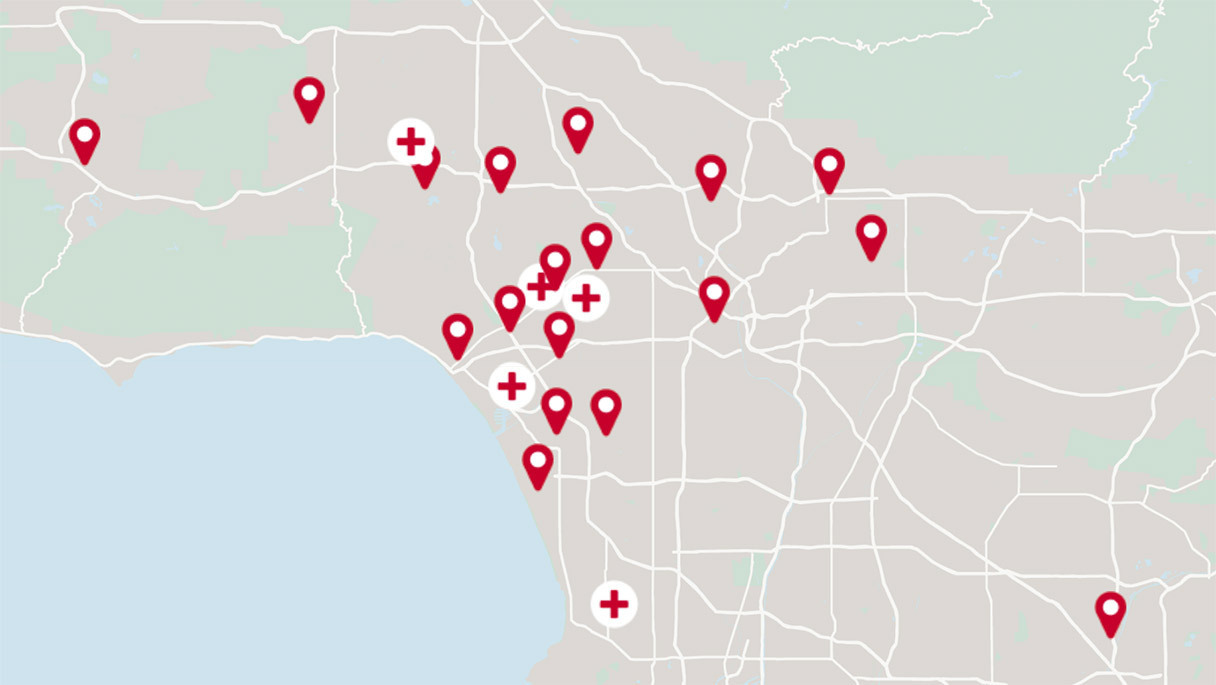
Cedars-Sinai has a range of comprehensive treatment options.
Get the care you need from world-class medical providers working with advanced technology.