Research Areas
- Magnetic Resonance Multitasking for Motion-Resolved Quantitative Cardiovascular Imaging
- International Whole-Brain Vessel Wall Imaging-Based Stroke Registry to Investigate Etiologies of Ischemic Stroke
- ECG and Navigator-Free 4-D Whole-Heart Coronary Magnetic Resonance Angiography
- Optimized Cardiac CEST MRI for Assessment of Metabolic Activity in the Heart
- Improving Noninvasive Therapy Evaluation of Stem-Cell-Based Treatment for Heart Failure with Diffusion Tensor MRI
- Noninvasive Measurement of Pressure Gradient across a Coronary Stenosis Using Phase-Contrast (PC)-MRI
- Coronary Atherosclerosis T1-Weighted Characterization with Integrated Anatomical Reference
- Ungated, Free-Breathing T1 Mapping
Improving Noninvasive Therapy Evaluation of Stem-Cell-Based Treatment for Heart Failure with Diffusion Tensor MRI
Introduction
Heart disease is the leading cause of death in the world. Advance noninvasive imaging techniques are sought out to guide and assess the efficacy of novel therapies to repair the heart such as exosomes from cardiosphere-derived cells (CDC-XO), developed by Eduardo Marbán, MD, PhD. One key advanced imaging tool developed by our group is Diffusion Tensor MRI (DTI) that can reveal the heart’s underlying fiber architecture. Applying DTI in the heart is technically challenging because of its inherent sensitivity to bulk motion, which in a moving organ like the heart is substantial. We aim to address these technical challenges, thereby yielding new, unique insight into evaluation of CDC-XO therapy.
Methods
To address the inherent motion sensitivity, we developed a second-order motion compensation gradient moment nulling (M2) that rephases the deleterious bulk motion-induced phase shifts. Without M2, these phase shifts will destroy the desired diffusion MRI contrast, resulting in signal voids. Further development was also made in the MRI readout employing a novel diffusion preparation scheme that allows for 3-D high-resolution.
This newly designed sequence was applied in 12 porcine with myocardial infarction in a randomized placebo controlled study to evaluate how the myocardial fiber orientations (HAT: helix angle transmurality) derived from DTI were affected by the CDC-XO treatment. Conventional MRI used to measure scar size (SS) and cardiac function (EF) was also acquired.
Results
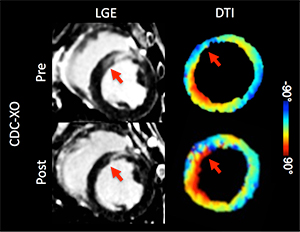
In the CDC-XO group (Figure 1), conventional MRI (LGE) revealed decreased SS (red arrow), and in the same region of reduced scar, DTI showed regrowth of the tissue realigning (blue to red) to surrounding tissue. Overall, the CDC-XO group demonstrated no significant change in HAT and a significant reduction in SS, representing a halt in disease progression. In the placebo group, both SS and HAT significantly changed in an adverse manner, reflecting disease progression. Receiver operator characteristic (ROC) curves (Figure 2) demonstrated that combined SS and HAT (0.93) had significantly improved prediction of the therapeutic endpoint EF in comparison to either SS (0.76) or HAT (0.82) alone.
Discussion
Our preliminary results in porcine show that CDC-XO treatment is not only reducing scar but also re-growing viable tissue that has partially realigned with the normal tissue. This effectively results in an overall halt to the disease progression of myocardial infarction. Furthermore, we have demonstrated that DTI has added value in predicting the therapeutic end point of cardiac function when combining it with conventional MRI. With the development of a robust DTI technique for the heart, cardiologists at Cedars-Sinai can potentially characterize the progression of heart disease in their patients and monitor the use of the novel therapies developed in their laboratories.
Conclusion
We developed a robust in-vivo cardiac DTI sequence capable of imaging in a clinical setting by overcoming major technical challenges. We also demonstrated DTI has added value in improving the prediction of the therapeutic efficacy of stem cell-based treatments.
Investigators
- Christopher T. Nguyen, PhD
- James Dawkins, DVM
- Eduardo Marbán, MD, PhD
Internal Collaborations
International Whole-Brain Vessel Wall Imaging-Based Stroke Registry to Investigate Etiologies of Ischemic Stroke
Introduction
Cedars-Sinai is sponsoring a new international multicenter vessel wall imaging-based stroke registry under the leadership of Zhaoyang Fan, PhD, Qi Yang, MD, PhD, and Debiao Li, PhD. The Whole Brain Vessel Wall Imaging in Stroke Patients (WISP) study will investigate the clinical utility of whole-brain vessel wall MRI in assessing the etiologies and stratifying risk in patients with recent ischemic stroke.
Stroke is a leading cause of mortality and morbidity worldwide and arises from different intracranial wall pathologies, such as atherosclerosis, vasculitis, dissection and Moyamoya disease. Accurate characterization of these pathologies, which is not provided by conventional imaging methods, may help elucidate stroke etiology and allow for therapeutic intervention before more severe cerebrovascular events occur.
Methods
The WISP study aims to provide a systematic data collection and analysis regarding the real clinical value of a novel whole-brain vessel wall MRI technique. The study population includes patients with a recent ischemic stroke within eight weeks and primary outcome measure is identification of pathologies such as atherosclerosis, dissection and vasculitis. A total of 1,000 subjects will be recruited through 2019 in a total of 12 centers in the U.S. and China.
Investigators
- Zhaoyang Fan, PhD
- Qi Yang, MD, PhD
- Debiao Li, PhD
- Marcel Maya, MD
- Konrad Schlick, MD
- Oana Dumitrascu, MD
- Shlee Song, MD
Internal Collaborations
- Neurology Department Comprehensive Stroke Center
- S. Mark Taper Foundation Imaging Center
- Fan Z, Yang Q, Deng Z, Li Y, Bi X, Song S, Li D. Whole-brain intracranial vessel wall imaging at 3 Tesla using cerebrospinal fluid-attenuated T1-weighted 3D turbo spin echo. Magn Reson Med. 2017 Mar;77(3):1142-1150.
- Yang Q, Deng Z, Bi X, Song SS, Schlick KH, Gonzalez NR, Li D, Fan Z. Whole-brain vessel wall MRI: A parameter tune-up solution to improve the scan efficiency of three-dimensional variable flip-angle turbo spin-echo. J Magn Reson Imaging. 2017 Sep;46(3):751-757.
- Wang W, Yang Q, Li D, Fan Z, Bi X, Du X, Wu F, Wu Y, Li K. Incremental value of plaque enhancement in patients with moderate or severe basilar artery stenosis: 3.0 T high-resolution magnetic resonance study. Biomed Res Int. 2017;2017:4281629.
- Wu F, Song H, Ma Q, Xiao J, Jiang T, Huang X, Bi X, Guo X, Li D, Yang Q, et al. Hyperintense plaque on intracranial vessel wall magnetic resonance imaging as a predictor of artery-to-artery embolic infarction. Stroke. 2018 Apr;49(4):905-911.
- Wang M, Wu F, Yang Y, Miao H, Fan Z, Ji X, Li D, Guo X, Yang Q. Quantitative assessment of symptomatic intracranial atherosclerosis and lenticulostriate arteries in recent stroke patients using whole-brain high-resolution cardiovascular magnetic resonance imaging. J Cardiovasc Magn Reson. 2018 Jun 7;20(1):35.
- Zhang N, Zhang F, Deng Z, Yang Q, Diniz M, Song SS, Schlick KH, Maya MM, Gonzalez N, Li D, et al. 3D whole-brain vessel wall cardiovascular magnetic resonance imaging: a study on the reliability in the quantification of intracranial vessel dimensions. J Cardiovasc Magn Reson. 2018 Jun 14;20(1):39.
- Wu F, Ma Q, Song H, Guo X, Diniz M, Song S, Gonzalez N, Bi X, Ji X, Li D, et al. Differential Features of Culprit Intracranial Atherosclerotic Lesions: A Whole-Brain Vessel Wall Imaging Study in Patients With Acute Ischemic Stroke. J Am Heart Assoc. 2018 Jul 22;7(15). pii: e009705.
- Zhang Z, Fan Z, Kong Q, Xiao J, An J, Li D, Yang Q, Zhuo Y. Visualization of the lenticulostriate arteries at 3T using black-blood T1-weighted intracranial vessel wall imaging: comparison with 7T TOF-MRA. Eur Radiol. 2018 Aug 27.
Optimized Cardiac CEST MRI for Assessment of Metabolic Activity in the Heart
Introduction
Adenosine triphosphate (ATP) is the essential energy source of myocardial contraction. The synthesis of myocardial ATP involves the conversion of phosphocreatine to creatine catalyzed by creatine kinase. It has been previously shown that cardiac dysfunction is associated with myocardial ATP loss.
CEST has been used to map creatine distribution in the myocardium to assess metabolic activity in animal models. However, the previous approach requires a lengthy scan time (50 minutes), which needs to be reduced considerably for human application.
Methods
In order to apply the cardiac CEST imaging technique for a clinical setting, the technique was optimized in the following aspects:
- Images were acquired by single-shot FLASH instead of segmented acquisition, resulting in an imaging time of four to five minutes, depending on the navigator acceptance rate.
- All images were registered using advanced normalization tools (ANTs) to further reduce the residual respiratory motion (up to four millimeter myocardium displacement). This helps improve the robustness of the cardiac CEST technique, especially since pixel-by-pixel mapping was performed afterward.
- Z-spectrum was fitted to the Lorentzian-shaped three-pool model to generate a CEST contrast map. This fitting method helps increase the reliability of the generated CEST contrast map by reducing the impact of signal fluctuation from B0 field shifting and residual motion.
Results
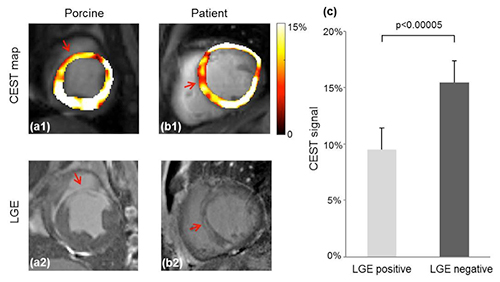
The figure below (a-b) shows representative CEST contrast maps and corresponding LGE images in porcine and the patient. The hypointense region in the CEST contrast map matches the bright area in the LGE image closely, suggesting that the scar region has reduced creatine distribution and lower metabolic activity compared to healthy myocardium. This is consistent with previous study.
Figure below (c) quantitatively compares the CEST signals in the LGE positive and negative regions in base, mid and apex slices in the porcine model. The CEST signal is significantly reduced in the infarct region (9.5 percent ± 1.9 percent), compared to healthy remote myocardium (15.5 percent ± 2.2 percent), p<0.00005. In the patient, CEST signal in the infarct region is 8.4 percent, while that in the healthy myocardium is 16.2 percent.
Conclusions
Our study also shows the feasibility of cardiac CEST imaging in a clinical setting. We can potentially apply this technique to detect metabolic abnormalities for cardiac dysfunction in patients.
Investigators
- Zhengwei Zhou
- Yuhua Chen, PhD
- Yibin Xie, PhD
- Christopher T. Nguyen, PhD
- James Dawkins, DVM
- Zhanming Fan, PhD
- Eduardo Marbán, MD, PhD
- Debiao Li, PhD
Internal Collaborations
External Collaborations
- Department of Radiology, Anzhen Hospital, Capital Medical University, Beijing, China
Representative Publications
- Haris M, Singh A, Cai K, Kogan F, McGarvey J, Debrosse C, Zsido GA, Witschey WRT, Koomalsingh K, Pilla JJ, et al. A technique for in vivo mapping of myocardial creatine kinase metabolism. Nat Med. 2014;20(2):209-214. http://www.nature.com/nm/journal/v20/n2/full/nm.3436.html.
- Dzeja PP, Redfield MM, Burnett JC, Terzic A. Failing energetics in failing hearts. Curr Cardiol Rep. 2000;2(3):212-217. http://link.springer.com/article/10.1007%2Fs11886-000-0071-9.
- Bottomley PA, Weiss RG. Non-invasive magnetic-resonance detection of creatine depletion in non-viable infarcted myocardium. Lancet. 1998;351(9104):714-718. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(97)06402-7/abstract.
- Sanbe A, Tanonaka K, Hanaoka Y, Katoh T, Takeo S. Regional energy metabolism of failing hearts following myocardial infarction. J Mol Cell Cardiol. 1993;25(9):995-1013. http://www.jmmc-online.com/article/S0022-2828(83)71113-2/abstract.
Noninvasive Measurement of Pressure Gradient across a Coronary Stenosis Using Phase-Contrast (PC)-MRI
Introduction
In patients suspected of coronary artery disease (CAD) undergoing invasive coronary angiography (ICA), ~50 percent has nonsignificant stenosis (<50 percent diameter stenosis or fractional flow reserve, FFR>0.80), resulting in unnecessary invasive procedures. This work aims to investigate the feasibility of a noninvasive technique to derive pressure difference across a coronary stenosis, with the ultimate goal of estimating FFR. The technique may have the potential for noninvasive assessment of the functional significance of coronary artery stenosis, for better risk stratification of patients with the likelihood of CAD prior to invasive catheterization.
Methods
The proposed technique uses 3-D velocities acquired using 2-D phase-contrast (PC)-MRI in conjunction with the Navier-Stokes equations to derive pressure difference across a coronary stenosis. The pressure difference across the lesion of interest was then converted to an MR-iFR index and compared to invasive FFR in patients to evaluate the feasibility of the technique.
Results
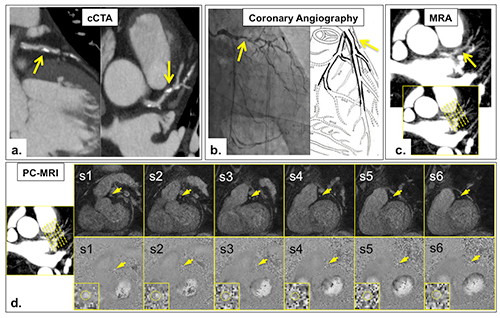
Good correlation (r=0.80; R2=0.64 (p<0.0001)) was observed between MR-iFR and FFR (Figure 1). Using an invasive FFR and MR-iFR (based on invasive iFR literature value) cut-off of 0.80 and 0.90, respectively, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were 75 percent, 95 percent, 75 percent and 95 percent, respectively. A representative figure in a patient with a functionally significant coronary stenosis is shown in Figure 2.
Conclusion
Preliminary studies demonstrated the feasibility of using PC-MRI derived pressure difference measurements for noninvasive assessment of coronary artery lesions. High specificity and NPV were observed, demonstrating the potential of the proposed technique in identifying patients with functionally nonsignificant stenosis. However, more patient studies with positive invasive FFRs are needed to further investigate the sensitivity of the approach, and further technical development in higher spatial-resolution and shorter scan time is needed to improve the accuracy and robustness of the technique.
Investigators
- Zixin Deng
- Zhaoyang Fan, PhD
- Sang-Eun Lee
- Xiaoming Bi
- Byoung-Wook Choi
- Jung-Sun Kim
- Daniel S. Berman, MD
- Hyuk-Jae Chang
- Debiao Li, PhD
Internal Collaborators
External Collaborators
- Severance Hospital, Seoul, South Korea
- Magnetic Resonance Research & Development, Siemens Healthcare, Los Angeles, CA
Representative Publications
- Deng Z, Lee SE, Fan Z, Nguyen C, Cho I, Yang Q, Bi X, Choi BW, Berman D, Chang, HJ, Li D. Pressure gradient measurement in the coronary artery using phase contrast (PC)-MRI: initial patient results toward noninvasive quantification of fractional flow reserve. J Cardiovasc Magn Reson. 2016;18(Suppl 1):P218. https://jcmr-online.biomedcentral.com/articles/10.1186/1532-429X-18-S1-P218.
- Let It Flow Session, Oral, ISMRM 23rd Annual Meeting & Exhibition. 2015 June. http://www.ismrm.org/15/program_files/TueSci15.htm
Contact the Li Lab
Cedars-Sinai Biomedical Imaging Research Institute
8700 Beverly Blvd.
Pacific Theaters 800
Los Angeles, CA 90048