October 2020 Case
Authors
David Negrete, MD, (Resident), Kevin Waters, MD, PhD (Faculty/Mentor)
Gastrointestinal Pathology
Clinical History
A male patient in his 40s with no significant past medical history presented with a one-month history of intermittent melena and anemia. He underwent wireless capsule enteroscopy which showed inflammatory-appearing small bowel lesions concentrated in the mid-ileum. Subsequent retrograde double balloon enteroscopy showed two small bowel tumors (0.7-1.5 cm) in the mid-ileum. CT showed a large empyema, a 2.6 cm T10 paravertebral mass (likely neurogenic mass), and a 2.3 cm soft tissue mass posterior to the anterior abdominal wall (believed to be a lipoma intraoperatively). Biopsies were taken of mid-ileal masses and a subsequent small bowel resection and pleural excision was performed.
Histology
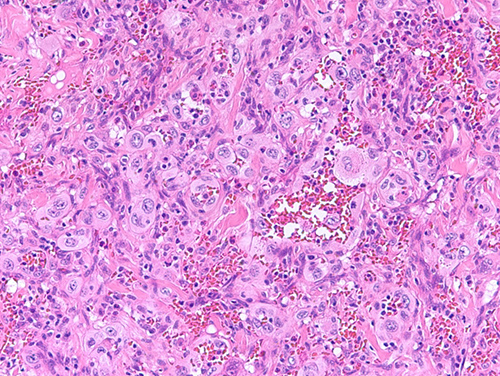
Figure 1: Section of small intestine tumor showing a predominately solid proliferation of large round to polygonal epithelioid cells with abundant eosinophilic cytoplasm, vesicular nuclei, central nucleoli, and frequent mitoses. Extravasated blood and vascular spaces are also evident.
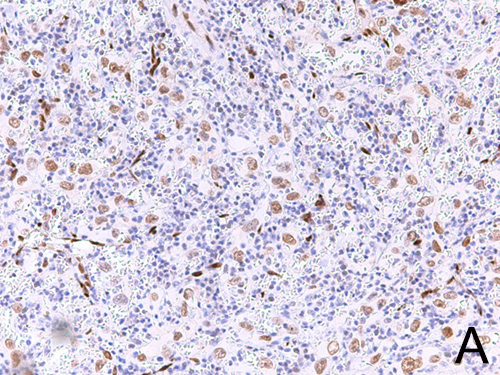
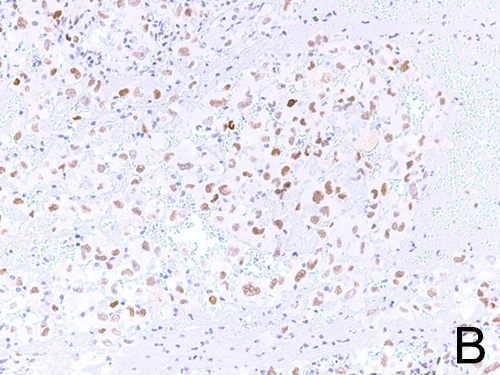
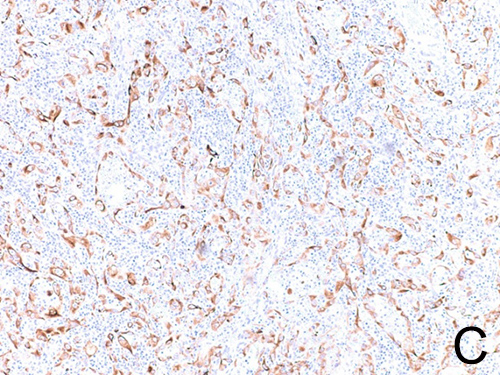
Figure 2. (A) The tumor shows positive nuclear staining for the endothelial marker, ERG. (B) Positive nuclear staining for cMYC and (C) positive cytoplasmic staining for cytokeratin (OSCAR) in tumor cells.
Diagnosis
Epithelioid angiosarcoma, high grade, involving small bowel and pleura
Discussion
Angiosarcomas are rare (<1-2% of sarcomas) and aggressive tumors showing morphologic and/or immunophenotypic evidence of vascular differentiation. They most often occur in the skin and subcutaneous tissues but can develop anywhere in the body due to the ubiquity of blood vessels. Epithelioid angiosarcoma (EAS) is an especially aggressive variant with a very poor prognosis. Within 2-3 years of diagnosis, more than 50% of patients succumb to disease. The most common presentation is an older individual (70s) with a deep soft tissue mass in the extremity.
Diagnosis can be difficult on histomorphology alone. The tumor can be mistaken for a (metastatic) carcinoma, lymphoma or malignant melanoma, making immunohistochemistry invaluable in final diagnosis. EAS often shows abnormal cytokeratin staining, one potential diagnostic pitfall. Unlike carcinomas, however, positivity for endothelial markers, including ERG, CD31, and CD34 should be apparent. Negative CD45 and CD30 staining can help exclude an anaplastic large cell lymphoma. EAS is also negative for S100, HMB-45, and Melan-A helping to rule out melanoma. The tumors in the current case stained positive for vascular markers ERG, CD31, and showed patchy cytokeratin positivity. A less aggressive vascular malignancy that should also be included in the differential is epithelioid hemangioendothelioma (EHE). CAMTA-1, a highly sensitive and specific marker for EHE, was negative in the current case, supporting a final diagnosis of EAS. MYC amplification is a typical finding in post-irradiation and chronic lymphedema-associated angiosarcomas (secondary angiosarcomas). However, it has been recently seen in a subset of primary tumors including cutaneous and hepatic angiosarcomas.
Tumors of the small intestine are rare, and angiosarcomas arising here are even more rare. However, primary small intestine angiosarcomas have been documented, including a multifocal presentation of primary EAS involving the small intestine. Surgical resection followed by adjuvant radiotherapy is the main treatment option for localized EAS. The current case unfortunately showed metastasis to one of six lymph nodes as well as pleural involvement, and the patient received adjuvant chemotherapy. Per imaging, no definitive mass beyond the small bowel suggested an alternative primary site. Considering the current clinical and pathologic findings, this may represent a multifocal presentation of primary small intestine EAS.
References
- Jesse Hart, Srinivas Mandavilli. Epithelioid Angiosarcoma: A Brief Diagnostic Review and Differential Diagnosis. Arch Pathol Lab Med 1 February 2011; 135 (2): 268–272.
- V. Delvaux et al. Multifocal epithelioid angiosarcoma of the small intestine. Virchows Archiv 1999; 437:90-94.
- Cao J, Wang J, He C, Fang M. Angiosarcoma: a review of diagnosis and current treatment. Am J Cancer Res. 2019;9(11):2303-2313.
- Ni, Q., Shang, D., Peng, H. et al. Primary angiosarcoma of the small intestine with metastasis to the liver: a case report and review of the literature. World J Surg Onc 11, 242 (2013).
- Pang, M., Gomez, V., Mittra, A., Krishna, M., Stark, M. Epithelioid Angiosarcoma: A Rare Culprit of Small Bowel Overt Bleeding, American Journal of Gastroenterology: October 2016 - 111: p S1068.
- Zemheri, E., Engin, P., Ozkanli, S., Ozemir, I.. Primary Angiosarcoma of Small Intestine Presenting With Intestinal Perforation: A Case Report. Journal of Medical Cases, North America, 5, Jan. 2014; 5(2), pp113-7.
- Nai Q, Ansari M, Liu J, et al. Primary Small Intestinal Angiosarcoma: Epidemiology, Diagnosis and Treatment. J Clin Med Res. 2018;10(4):294-301.
- Shon, W., Sukov, W., Jenkins, S. et al. MYC amplification and overexpression in primary cutaneous angiosarcoma: a fluorescence in-situ hybridization and immunohistochemical study. Mod Pathol 27, 509–515 (2014).